Introduction
The last European LeukamiaNet (ELN) recommendations (Döhner H. et al. Blood. 2022) and the International Consensus Classification (ICC, Hasserjian R.P. et al. Virchows Arch. 2023) described a new entity, called myelodysplastic syndrome (MDS)/ acute myeloid leukemia (AML) with TP53 mutation ( TP53mut), comprising high-risk MDS with an excess of bone marrow blasts cells (more than 10%) and a TP53 mutation (variant allele frequency VAF ≥ 10%). They suggested that MDS and AML represent a biologic continuum rather than two distinct diseases separated by a blast cutoff. Among teams who worked on that topic, T. Grob et al. ( Blood. 2022) studied the molecular characterization of high-risk AML and MDS with TP53mut and suggested that these two types of pathologies should be considered as a single entity, with no difference in molecular characteristics or survival. In this study, we describe the clinical, cytogenetic, and molecular characteristics of a cohort of 96 MDS and AMLs with TP53mut.
Patients and methods
We included all the patients with AML, MDS/AML, MDS with increased blasts (MDS-IB1) and MDS-low blast (MDS-LB) with at least one TP53mut (VAF ≥ 1%) received between Aug. 2020 and Dec. 2022 at the Institut Paoli-Calmettes (IPC, Marseille, France). Clinical and biological data were extracted retrospectively from the AML IPC database. Morphologic and cytogenetic data were analyzed by standard techniques. NGS was performed using a custom targeted panel of 60 genes (Custom Myeloid Lymphoid Solution, SOPHIA GENETICS).
Results
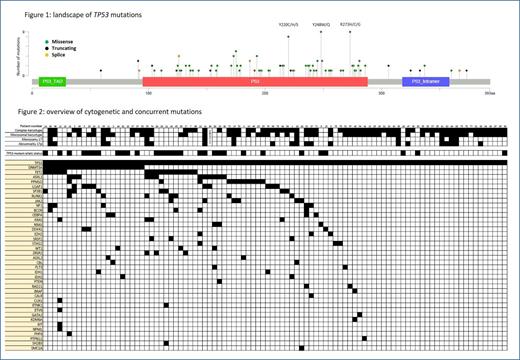
We registered 96 patients with a TP53 mutation (VAF ≥ 1%), divided into AML (n=60), MDS/AML (n=14), MDS-IB1 (n=12) and MDS-LB (n=10). Median age was 71 (range, 28-88). Thirty-eight patients had been treated for a prior solid malignancy and 26 patients had a history of myeloid malignancy. TP53mut was detected at diagnosis for 85 patients and at relapse or during follow-up for 12 patients (no NGS data available at diagnosis). We detected 142 mutations in the TP53 gene, mostly missense (73%) between exon 4 and exon 11 with a median VAF of 39% (Figure 1). We found 3 hotspots mutations in positions 273, 248 and 220 with respectively 9, 9 and 8 mutations. Biallelic status (presence of ≥ 2 mutations or a mutation + a deletion) was found in 66 patients (69%). Karyotypes were available for 95 patients. The karyotype was abnormal in 88% of cases, complex in 71% and unfavorable in 80% of cases according to ELN classification or Revised International Prognostic Scoring System (R-IPSS). Complete NGS analysis revealed at least one mutation in 59 of the other genes of the panel in 67 patients (70%), the most frequent being DNMT3A (22%), TET2 (17%), ASXL1 (13%) and PPM1D (11%) (Figure 2). In our cohort of TP53mut LB-MDS (n=10), we found that 9/10 patients had co-mutations in DNMT3A (n=4) , TET2 (n=6) and PPM1D (n=2) genes, 7/10 with biallelic status and 3/10 with complex karyotype. AML and MDS/AML patients with TP53mut detected at diagnosis (n=65) were treated with intensive chemotherapy (n=13), VEN-AZA (n=26), non-intensive therapy (n=14) or best supportive care (BSC, n=12). Seventeen patients were treated with allogeneic stem-cell transplantation (ASCT). With a median follow-up (FU) of 13 months, median overall survival (OS) of the whole cohort was 7 months (ranges, 1-41). Median OS in the AML and MDS/AML group was 6 months (ranges, 1-41). Patients treated with non-intensive approach had the longest median OS (15 months) compared to patients treated with intensive chemotherapy and VEN-based approaches (8 and 6 months, respectively) and patients treated with BSC (1 month, p=0.02). Patients with MDS-IB1 and MDS-LB had 11-months median OS (ranges, 1-28). The four patients treated with upfront ASCT were still alive at the last FU date and have an estimated median OS of 18.5 months (ranges, 6-26).
Conclusion
Our data confirm that MDS and AML with TP53 mutation are frequently associated with complex karyotypes and have a poor prognosis. nterestingly we identified mutations in PPM1D gene, involved in TP53 pathway, in 11% of cases. Patients with AML or MDS/AML treated with non-intensive approach seem to have the longest OS (15 months). Patients with MDS-IB1 or MDS-LB treated with upfront ASCT seem to have a prolonged OS (18.5 months). Clinical, functional and mechanistic studies are required to complete these findings.
Disclosures
Charbonnier:Pfizer, Novartis, Incyte Biosciences: Honoraria. Devillier:Astellas: Honoraria; Incyte: Honoraria; Jazz Pharmaceuticals: Honoraria; Medac: Honoraria; Sanofi: Honoraria; MSD: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal